Living with Parkinson’s Disease (PD) can be challenging to say the least. As the condition progresses, it often requires the a continuous adoption of new strategies and treatments to help manage its symptoms.
In my personal journey with PD, I have remained open-minded to a wide range of traditional and homeopathic therapies and medications including: yoga, isometrics, stretching, chiropractic, acupuncture, massage, supplements, vitamins, hyperbaric chamber, IV fusion Muscle Activation Techniques (MAT), and mental and physical counseling – all with the goal of improving my quality of life.
While these treatments provided some temporary relief, each of them ultimately became less effective over time. In a way, it was like trying to hit a moving target.
In 2020, I had a major breakthrough after partaking in a procedure that combines neuroscience and medical technology known as Deep Brain Stimulation (DBS).
What is Deep Brain Stimulation (DBS)?
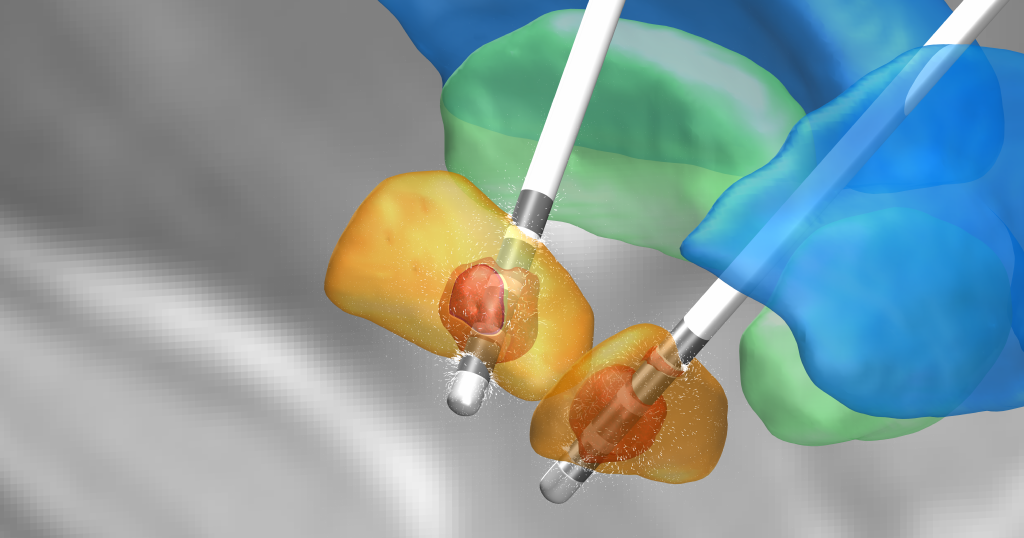
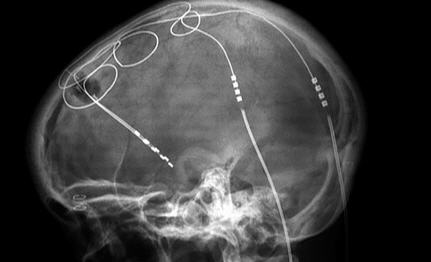
To me, Deep Brain Stimulation is like having a heart pacemaker for the brain. DBS is a surgical procedure that involves the placement of a thin wire or electrode in the damaged area(s) of the brain. The wire is connected to a medical device implanted under the skin near the collarbone. Once activated, the device sends electrical impulses through the wire to the targeted area(s) of the brain to help:
- Reduce medication “Off” times
- Improve quality of life
- Reduce symptoms
- Increase independence
The latest generation of DBS is adjustable and reversible. New technology allows doctors and patients to adjust via remote control the optimum level of relief with the least side effects.
My Personal Experience with DBS
In 2019, the Carbidopa/Levodopa medication I was taking to control my symptoms began to lose its effectiveness. It got to the point where I had to time my daily activities around the anticipated “On/Off” times of the medication. This randomness of my medication also began taking a toll on my mental well-being, as I developed anxiety, which I never experienced before. As the months progressed, my symptoms continued to worsen and my quality of life and world was literally shrinking right before my eyes.
By February 2020, I was having difficulty functioning independently. Simple activities such as going to the grocery store, became a perceived mental and physical challenge. At the encouragement of a good friend, I went to the Penn State/Milton Hershey Medical Center Emergency Room for an evaluation. After two days, I checked myself out and upon returning home, my body completely shut down. I refer to this as my PTSD moment, because I could no longer stand, walk or do anything on my own.
For the next three months, I received 24×7 care from a local home care provider along with the support of friends and family. During this time, I slowly began to regain some basic daily life functions, primarily through medication trial and error, perseverance and faith. At the same time, I began to realize that my only hope for having any type of a normal quality of life going forward was to have the DBS procedure.
A very close friend and his wife and I began investigating the DBS procedure and potential outcomes I could anticipate. This information gave me a renewed my sense of hope and optimism. Having said this, DBS is not for everyone and I would encourage anyone considering this procedure to consult with both a neurologist and neurosurgeon early on in the research process. After consulting with multiple neurologists, I was recommended as a potential candidate for the DBS procedure.
One of the memorable moments in this exhaustive process, came about when neurologist Dr. Venkatachalam Mangeshkumar was comparing the current MRI scan to the original scan in 2007, and commented that the 2020 scan showed little deterioration in the brain over the last 13 years. This came as a complete surprise to the three of us because we didn’t know what to expect after this period of time.
In April 2020, I had a DBS telephone consult and office visit with neurosurgeon, Dr. Steven Falowski, in which he reviewed the procedure and addressed questions that we had compiled regarding the technology and the anticipated post-DBS procedure benefits. We felt that Dr. Falowski presented the pros and cons of the DBS procedure in a manner that was both real and direct. We were especially impressed with the fact that Dr. Falowski had performed over 1,000 procedures under the guidance of the inventor of the initial procedure.
Preparing for the DBS Procedure
My pre-DBS surgery included a series of both office visits and telephone consultations with a team of DBS support personnel. This process included cognitive testing to determine:
- Memorization of a series of numbers, lists of animals, phrases etc.
- Reading comprehension
- Shape cognition and complex math problems
In September, the UPMC neurology practice was going through a transition so Dr. Falowski referred me to a highly respected professional colleague Dr. James McInerney of PS/MSHMC to perform my procedure. I had an introductory telephone consult with Dr. McInerney and a pre-surgery appointment to mark the fixed head locations for the surgery.
In November, Dr. McInerney performed the initial brain surgery and then several weeks later he installed the generator near my collarbone. After the holidays, I went back to have Dr. DeJesus and her staff program the DBS system for me. What was really impressive to me was how I felt the effects her tweaking the system immediately on my right arm.
Going into the surgery, we were hoping to reduce the cramping in my left foot, improve the gait issue with my right leg, reduce my medication On/Off transition times (creating a floor for my symptoms) and to help me regain my confidence and fluidity of movement.
Post-DBS Outcome
I am happy to say that the DBS procedure exceeded our expectations in all areas and marked a new chapter in my life, improving my mental, physical, and spiritual well-being. After such a long period of challenges, I finally felt like I was returning to the best version of myself. Even my friends and family have noticed the positive changes after my DBS procedure. Since then, I have fully resumed my daily activities and have continue to move forward with a restored sense of wellbeing.
Deep Brain Stimulation stands as a testament to the advancements in neurology and surgical interventions for the treatment of PD. For me, it’s been more than a treatment, it’s been a path to reclaiming my quality of life.
Disclaimer: This information is for general knowledge only and should not be used in place of professional medical advice. This is my personal story and understanding. Always consult with your doctor or a qualified healthcare provider for advice.